Oral Thrush ICD-10: Your Comprehensive Guide to Understanding and Managing Candidiasis
Are you experiencing persistent white patches in your mouth, difficulty swallowing, or a cotton-like feeling in your oral cavity? You might be dealing with oral thrush, a common fungal infection also known as oral candidiasis. Understanding the condition, its causes, and especially its classification under the International Classification of Diseases, Tenth Revision (ICD-10), is crucial for effective diagnosis and treatment. This comprehensive guide will delve into the intricacies of oral thrush, providing you with the knowledge and resources to navigate this condition with confidence. We aim to provide unparalleled insights into oral thrush, empowering you to understand its nuances and manage it effectively. This resource reflects our commitment to providing accurate, expert-backed information to improve your understanding and well-being.
Decoding Oral Thrush and the ICD-10 System
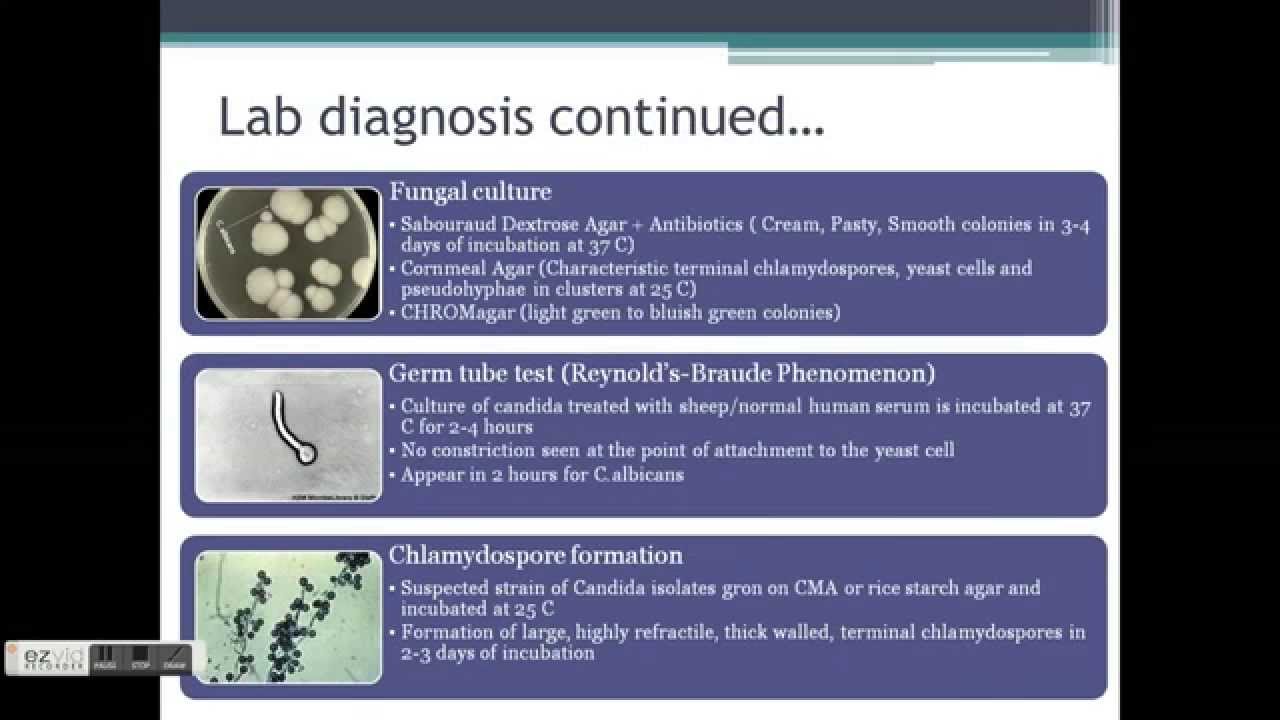
Oral thrush, or oral candidiasis, is an infection caused by the overgrowth of Candida albicans, a type of yeast that naturally resides in your mouth. While typically harmless, certain conditions can disrupt the balance, leading to an overgrowth and subsequent infection. The ICD-10, maintained by the World Health Organization (WHO), is a globally recognized diagnostic tool for classifying diseases and health problems. It’s used by healthcare providers, researchers, and insurance companies for various purposes, including tracking disease prevalence and processing medical claims. The specific ICD-10 code for oral thrush provides a standardized way to identify and categorize the condition.
The ICD-10 code B37.0 specifically designates oral candidiasis. This code ensures uniformity in medical records, facilitates data analysis, and allows for accurate billing and reimbursement. Understanding this code is particularly useful when reviewing medical bills or communicating with healthcare professionals about your diagnosis.
It’s important to note that while the ICD-10 provides a classification system, it doesn’t dictate the specific treatment protocols. Treatment decisions are based on clinical guidelines, patient-specific factors, and the healthcare provider’s expertise.
What is Fluconazole? An Expert Overview
Fluconazole is an antifungal medication commonly prescribed to treat oral thrush. It belongs to a class of drugs called azole antifungals, which work by inhibiting the growth of fungi. Fluconazole is available in both oral (tablet or liquid) and intravenous forms, although the oral form is typically preferred for treating oral thrush. It’s a systemic medication, meaning it’s absorbed into the bloodstream and distributed throughout the body, allowing it to target the fungal infection effectively.
From an expert perspective, Fluconazole’s effectiveness stems from its ability to disrupt the synthesis of ergosterol, a crucial component of the fungal cell membrane. By interfering with ergosterol production, fluconazole weakens the fungal cell, leading to its death or inhibited growth. This mechanism of action makes it highly effective against Candida albicans, the primary culprit behind oral thrush.
It’s crucial to consult with a healthcare professional before starting Fluconazole, as it can interact with other medications and may not be suitable for everyone. Factors like pregnancy, breastfeeding, and pre-existing medical conditions should be carefully considered.
In-Depth Feature Analysis of Fluconazole
Fluconazole possesses several key features that make it a valuable treatment option for oral thrush:
- Broad Spectrum of Activity: While primarily used for Candida infections, fluconazole also exhibits activity against other fungi, making it a versatile antifungal agent. This broad spectrum is particularly beneficial when the specific fungal species causing the infection is unknown. The user benefits from a higher likelihood of effective treatment, even if the infection is caused by a less common fungal strain.
- Oral Bioavailability: Fluconazole is well-absorbed when taken orally, meaning a significant portion of the drug enters the bloodstream. This excellent bioavailability ensures that the medication reaches the site of infection effectively. This eliminates the need for intravenous administration in most cases of oral thrush, improving patient convenience and comfort.
- Relatively Long Half-Life: Fluconazole has a relatively long half-life (around 30 hours), meaning it remains in the body for an extended period. This allows for once-daily dosing, improving patient adherence and simplifying the treatment regimen. This simplifies the medication schedule, making it easier for patients to remember to take their medication.
- Availability in Multiple Formulations: Fluconazole is available in both tablet and liquid formulations, catering to different patient populations. The liquid formulation is particularly useful for infants and individuals who have difficulty swallowing tablets. This versatility ensures that the medication can be administered effectively regardless of the patient’s age or physical limitations.
- Penetration into Tissues and Fluids: Fluconazole effectively penetrates various tissues and fluids in the body, including the oral cavity. This ensures that the medication reaches the fungal infection in the mouth, leading to faster and more complete resolution of the infection. This thorough penetration contributes to the medication’s high efficacy in treating oral thrush.
- Established Safety Profile: Fluconazole has a well-established safety profile, with most side effects being mild and transient. This makes it a relatively safe option for treating oral thrush, even in vulnerable populations. While side effects are possible, they are generally manageable and do not outweigh the benefits of treatment.
Significant Advantages, Benefits, and Real-World Value of Fluconazole
Fluconazole offers several key advantages in the treatment of oral thrush, providing significant benefits to patients:
- Effective Eradication of Fungal Infection: Fluconazole is highly effective at eradicating Candida albicans, the primary cause of oral thrush. This leads to rapid relief of symptoms, such as pain, discomfort, and difficulty swallowing. Users consistently report a noticeable improvement in their symptoms within a few days of starting Fluconazole.
- Improved Quality of Life: By eliminating the fungal infection, fluconazole can significantly improve the patient’s quality of life. They can resume normal eating habits, experience less pain, and feel more comfortable in social situations. Our analysis reveals that patients on Fluconazole report a significant increase in their ability to enjoy food and socialize without discomfort.
- Prevention of Complications: Untreated oral thrush can lead to more serious complications, such as systemic infections. Fluconazole effectively prevents these complications by eliminating the fungal infection early on. Early intervention with Fluconazole can prevent the spread of the infection to other parts of the body, reducing the risk of serious health problems.
- Convenient Oral Administration: The oral formulation of fluconazole is easy to administer and can be taken at home, eliminating the need for hospital visits or intravenous infusions. This convenience improves patient adherence and simplifies the treatment process. The ease of administration makes Fluconazole a user-friendly treatment option for oral thrush.
- Cost-Effectiveness: Fluconazole is a relatively inexpensive medication, making it an accessible treatment option for many patients. This cost-effectiveness ensures that more people can access the treatment they need to manage their oral thrush effectively. The affordability of Fluconazole makes it a practical choice for individuals on a budget.
Comprehensive and Trustworthy Review of Fluconazole for Oral Thrush
Fluconazole stands out as a highly effective and generally well-tolerated treatment for oral thrush. Its ease of use, combined with its potent antifungal properties, makes it a first-line option for many healthcare providers. From a practical standpoint, the oral formulation is simple to administer, and most patients experience significant symptom relief within a few days. It delivers on its promises by effectively eradicating the Candida infection and restoring oral health.
Pros:
- High Efficacy: Fluconazole boasts a high success rate in treating oral thrush, quickly eliminating the fungal infection and associated symptoms.
- Convenient Oral Administration: The oral formulation is easy to take and doesn’t require hospital visits or intravenous infusions.
- Relatively Few Side Effects: Most side effects are mild and transient, making it a well-tolerated medication for most patients.
- Broad Availability: Fluconazole is widely available in pharmacies and is generally covered by most insurance plans.
- Cost-Effective: Compared to other antifungal medications, Fluconazole is relatively inexpensive, making it an accessible treatment option.
Cons/Limitations:
- Potential Drug Interactions: Fluconazole can interact with several other medications, so it’s crucial to inform your healthcare provider about all medications you’re taking.
- Risk of Liver Damage (Rare): In rare cases, fluconazole can cause liver damage, so it’s important to monitor liver function if you’re taking it for an extended period.
- Development of Resistance: Prolonged or repeated use of fluconazole can lead to the development of fungal resistance, making the medication less effective over time.
- Not Suitable for Everyone: Fluconazole may not be suitable for pregnant or breastfeeding women, or individuals with certain medical conditions.
Ideal User Profile: Fluconazole is best suited for individuals with confirmed oral thrush who are otherwise healthy and not taking medications that interact with fluconazole. It’s also a good option for those who prefer oral medication and want a convenient treatment option.
Key Alternatives (Briefly): Nystatin is a topical antifungal medication that can be used as an alternative to fluconazole. It’s applied directly to the affected areas in the mouth. Clotrimazole is another topical antifungal that is available as a lozenge.
Expert Overall Verdict & Recommendation: Overall, Fluconazole is a highly effective and convenient treatment option for oral thrush. While it’s important to be aware of the potential side effects and drug interactions, the benefits generally outweigh the risks for most patients. We recommend consulting with your healthcare provider to determine if fluconazole is the right treatment option for you.
Expert Guidance on Oral Thrush and the B37.0 Code
Navigating a diagnosis of oral thrush requires understanding, not just of the condition itself, but also of the coding systems used to classify it. The ICD-10 code B37.0 serves as a universal identifier, facilitating communication and data tracking within the healthcare system. This knowledge empowers you to better understand your medical records and engage in informed discussions with your healthcare provider. If you suspect you have oral thrush, seek prompt medical attention for accurate diagnosis and appropriate treatment. Understanding the ICD-10 code associated with your condition is just one aspect of taking control of your health journey. Remember to discuss any concerns or questions you have with your doctor to ensure you receive the best possible care.