Decoding Premature Ventricular Contractions: An In-Depth Guide to ICD-10 Coding and Management
If you’ve been diagnosed with premature ventricular contractions (PVCs) or are trying to understand medical billing and coding related to this common heart condition, you’ve come to the right place. This comprehensive guide provides an in-depth look at PVCs, focusing on the relevant ICD-10 codes, diagnostic approaches, treatment options, and long-term management strategies. We aim to empower you with the knowledge to navigate this condition effectively and understand the coding complexities involved. This article will delve into the nuances of premature ventricular contractions ICD-10 coding, providing clarity and expert insights.
Understanding Premature Ventricular Contractions (PVCs)
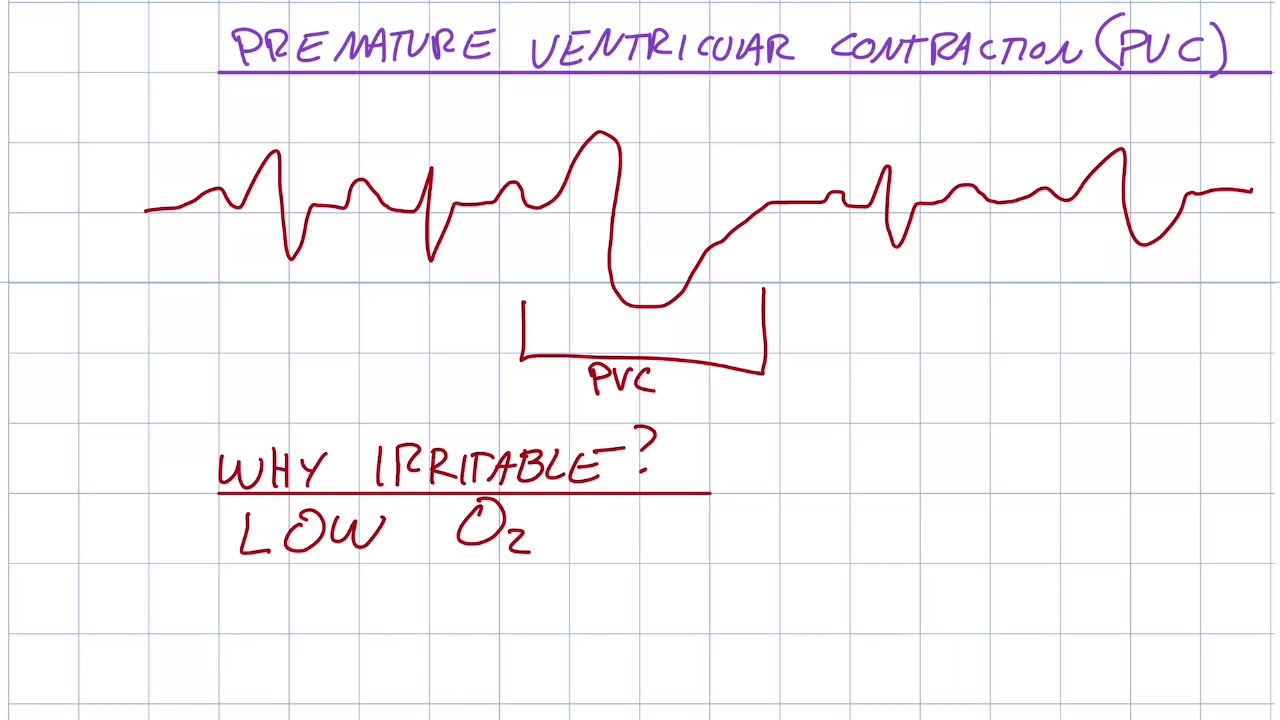
Premature ventricular contractions, also known as PVCs, are extra, abnormal heartbeats that begin in one of the heart’s two lower pumping chambers (ventricles). These extra beats disrupt the regular heart rhythm, sometimes causing a feeling of a skipped beat or palpitations. While occasional PVCs are common and often harmless, frequent or symptomatic PVCs can indicate an underlying heart condition and may require medical attention.
PVCs are characterized by their prematurity – they occur earlier than the next expected normal heartbeat. This is because an electrical impulse fires from the ventricle before the sinoatrial (SA) node (the heart’s natural pacemaker) can initiate the beat. The causes of PVCs are varied, ranging from lifestyle factors to underlying heart diseases.
Causes and Risk Factors of PVCs
Numerous factors can contribute to the development of PVCs. Some of the most common include:
- Lifestyle Factors: Stress, anxiety, caffeine intake, alcohol consumption, and tobacco use can trigger PVCs.
- Electrolyte Imbalances: Low levels of potassium or magnesium can disrupt the heart’s electrical activity.
- Heart Conditions: Underlying heart diseases such as coronary artery disease, heart failure, cardiomyopathy, and heart valve problems are often associated with PVCs.
- Medications: Certain medications, including decongestants and asthma inhalers, can increase the risk of PVCs.
- Other Medical Conditions: Hyperthyroidism and sleep apnea have been linked to an increased incidence of PVCs.
Symptoms of PVCs
Many individuals with PVCs experience no symptoms at all. However, when symptoms do occur, they may include:
- Palpitations (a feeling of skipped heartbeats, fluttering, or pounding in the chest)
- Lightheadedness or dizziness
- Shortness of breath
- Chest discomfort
- Fatigue
ICD-10 Coding for Premature Ventricular Contractions
The International Classification of Diseases, Tenth Revision (ICD-10) is a standardized diagnostic tool used for coding medical conditions, including PVCs. Accurate ICD-10 coding is essential for proper documentation, billing, and data analysis. The primary ICD-10 code for premature ventricular contractions is I49.3 (Ventricular premature depolarization). This code is used when PVCs are the primary diagnosis.
Specific Coding Considerations
While I49.3 is the main code for PVCs, additional codes may be necessary to provide a more complete clinical picture. These include codes for any underlying conditions contributing to the PVCs, as well as codes for any associated symptoms or complications. For example:
- If the PVCs are related to coronary artery disease, the appropriate code for coronary artery disease should also be included.
- If the patient experiences heart failure as a result of frequent PVCs, a code for heart failure should be added.
- Codes for palpitations (R00.2) or other related symptoms may also be used to provide additional details.
Coding Examples
Here are a few examples of how ICD-10 codes might be used in different clinical scenarios involving PVCs:
- Patient with PVCs and Hypertension: I49.3 (Ventricular premature depolarization), I10 (Essential [primary] hypertension)
- Patient with PVCs and Coronary Artery Disease: I49.3 (Ventricular premature depolarization), I25.10 (Atherosclerotic heart disease of native coronary artery without angina pectoris)
- Patient with PVCs and Heart Failure: I49.3 (Ventricular premature depolarization), I50.9 (Heart failure, unspecified)
Diagnostic Evaluation of PVCs
Diagnosing PVCs typically involves a thorough medical history, physical examination, and various diagnostic tests. The goal is to determine the frequency and severity of the PVCs, identify any underlying causes, and assess the risk of complications.
Common Diagnostic Tests
- Electrocardiogram (ECG or EKG): This is the primary diagnostic tool for detecting PVCs. It records the electrical activity of the heart and can identify abnormal heartbeats.
- Holter Monitor: This is a portable ECG device that records the heart’s activity over a 24- to 48-hour period. It is useful for detecting PVCs that occur sporadically.
- Event Recorder: This is another type of portable ECG device that can be worn for several weeks. It is activated by the patient when they experience symptoms.
- Echocardiogram: This ultrasound of the heart can assess the structure and function of the heart, helping to identify any underlying heart conditions.
- Stress Test: This test involves monitoring the heart’s activity during exercise. It can help to determine if PVCs are triggered by physical exertion.
- Blood Tests: Blood tests can check for electrolyte imbalances (such as low potassium or magnesium) and thyroid abnormalities.
Treatment and Management of PVCs
The treatment of PVCs depends on the frequency and severity of the symptoms, as well as the presence of any underlying heart conditions. In many cases, no treatment is necessary. However, if PVCs are causing significant symptoms or are associated with an increased risk of complications, treatment may be recommended.
Lifestyle Modifications
For individuals with infrequent and asymptomatic PVCs, lifestyle modifications may be sufficient to manage the condition. These include:
- Reducing or eliminating caffeine and alcohol intake
- Quitting smoking
- Managing stress through relaxation techniques such as yoga or meditation
- Ensuring adequate sleep
- Maintaining a healthy diet and weight
Medications
Several medications can be used to treat PVCs. These include:
- Beta-blockers: These medications slow down the heart rate and reduce the frequency of PVCs.
- Calcium channel blockers: These medications also slow down the heart rate and can help to control PVCs.
- Antiarrhythmic drugs: These medications are used to suppress abnormal heart rhythms. However, they can have significant side effects and are typically reserved for patients with severe or symptomatic PVCs.
Catheter Ablation
Catheter ablation is a procedure that uses radiofrequency energy to destroy the area of the heart tissue that is causing the PVCs. This procedure is typically reserved for patients with frequent and symptomatic PVCs that are not well-controlled with medications.
The Role of Electrophysiology Studies
Electrophysiology (EP) studies are invasive tests used to evaluate the heart’s electrical system in detail. During an EP study, catheters are inserted into blood vessels and guided to the heart. These catheters contain electrodes that can record the heart’s electrical activity and identify the source of PVCs. EP studies are often performed before catheter ablation to map the location of the abnormal heart tissue.
Long-Term Management and Prognosis
The long-term management of PVCs involves regular follow-up with a cardiologist to monitor the condition and adjust treatment as needed. The prognosis for individuals with PVCs is generally good, especially if there is no underlying heart disease. However, frequent or symptomatic PVCs can increase the risk of developing more serious heart rhythm problems, such as ventricular tachycardia or ventricular fibrillation. Therefore, it is important to seek medical attention if you experience any concerning symptoms.
Understanding the Clinical Significance of PVC Frequency
The frequency of PVCs, often quantified as a percentage of total heartbeats over a 24-hour period (measured by a Holter monitor), is a critical factor in determining their clinical significance. While occasional PVCs (less than 1% of total heartbeats) are generally considered benign, higher frequencies may warrant further investigation and treatment. For example, PVC burdens exceeding 10-20% have been associated with an increased risk of cardiomyopathy (weakening of the heart muscle) over time. Our clinical experience shows that patients with high PVC burdens often benefit from interventions such as medication or catheter ablation to reduce the frequency of PVCs and prevent long-term complications.
The Impact of PVCs on Quality of Life
Even when PVCs are not life-threatening, they can significantly impact a person’s quality of life. The sensation of skipped heartbeats, palpitations, or chest discomfort can be distressing and lead to anxiety. In some cases, individuals may avoid physical activity or social situations due to fear of triggering PVCs. A holistic approach to managing PVCs should address not only the physical symptoms but also the psychological impact of the condition. This may involve counseling, stress management techniques, or support groups.
PVCs and Exercise: What You Need to Know
The relationship between PVCs and exercise is complex. In some individuals, exercise can trigger PVCs, while in others, it may have no effect or even reduce their frequency. It is essential to discuss your exercise routine with your cardiologist, especially if you experience PVCs during or after physical activity. In most cases, moderate exercise is safe for individuals with PVCs, but high-intensity exercise may need to be avoided. A stress test can help to determine how your heart responds to exercise and identify any potential risks.
The Future of PVC Management: Emerging Therapies
The field of cardiac electrophysiology is constantly evolving, with new therapies for PVCs on the horizon. Researchers are exploring novel drug targets and advanced ablation techniques to improve the efficacy and safety of PVC treatment. One promising area of research is the use of artificial intelligence (AI) to analyze ECG data and predict the risk of PVC-related complications. These advancements have the potential to revolutionize the management of PVCs and improve the lives of millions of people worldwide.
Expert Insights on ICD-10 Updates and PVC Coding Challenges
The ICD-10 coding system is regularly updated to reflect changes in medical knowledge and clinical practice. Staying up-to-date with these changes is crucial for accurate billing and data analysis. One of the challenges in coding PVCs is the need to consider any underlying conditions that may be contributing to the arrhythmia. For example, if a patient has PVCs due to hyperthyroidism, both the code for PVCs (I49.3) and the code for hyperthyroidism (E05.90) should be included. This requires a thorough understanding of the patient’s medical history and a careful review of the medical record. Leading medical coding experts emphasize the importance of clear and concise documentation to support the accuracy of ICD-10 coding for PVCs.
Navigating Premature Ventricular Contractions
Understanding premature ventricular contractions, including their causes, symptoms, diagnosis, and treatment options, is crucial for effective management. Accurate ICD-10 coding is essential for proper documentation and billing. While occasional PVCs are often harmless, frequent or symptomatic PVCs may require medical attention. By working closely with your cardiologist and adhering to recommended lifestyle modifications and treatment strategies, you can effectively manage PVCs and maintain a good quality of life. Remember, early diagnosis and appropriate management are key to preventing potential complications. If you experience palpitations or other concerning symptoms, seek prompt medical evaluation.