Decoding ICD-10 Code Urinary Frequency: A Comprehensive Guide
Experiencing the sudden and frequent urge to urinate can be disruptive and concerning. Healthcare professionals rely on standardized coding systems to accurately document and diagnose medical conditions. When it comes to urinary frequency, the ICD-10 code plays a crucial role. This comprehensive guide delves into the intricacies of the ICD-10 code for urinary frequency, providing a thorough understanding of its definition, application, and implications. We aim to empower both healthcare providers and individuals seeking information about this common symptom.
Understanding Urinary Frequency and the ICD-10
Urinary frequency, also known as frequent urination, is the need to urinate more often than usual. What constitutes “normal” varies from person to person, but generally, needing to urinate more than eight times in a 24-hour period, while awake, might be considered frequent. The ICD-10, or International Classification of Diseases, Tenth Revision, is a globally recognized diagnostic coding system used to classify and code all diagnoses, symptoms, and procedures recorded in conjunction with hospital care in the United States. It’s essential for billing, research, and tracking health trends. When a patient presents with urinary frequency, the physician must determine the underlying cause. The specific ICD-10 code used will depend on the diagnosis, but codes related to urinary frequency are vital for documenting the symptom itself, particularly when a definitive diagnosis is not immediately available.
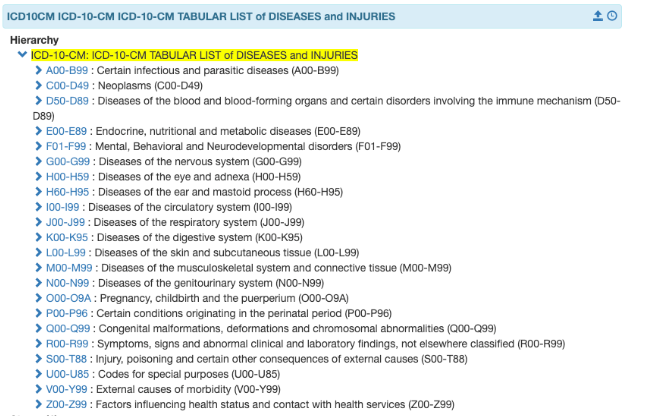
ICD-10-CM Coding: The Basics
ICD-10-CM stands for International Classification of Diseases, Tenth Revision, Clinical Modification. It is used to code diagnoses and reasons for encounters in all healthcare settings. Each code is alphanumeric and consists of 3 to 7 characters. The first character is a letter, and the second is a number. The remaining characters can be either letters or numbers. The ICD-10-CM coding system is updated annually by the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare & Medicaid Services (CMS).
Specific ICD-10 Codes Related to Urinary Frequency
While there isn’t one single ICD-10 code solely for urinary frequency, several codes might be applicable depending on the context and any associated conditions. It’s crucial to understand the nuances of each code to ensure accurate documentation. This is where a clinician’s experience is paramount. A common code used when urinary frequency is a presenting symptom is R35 (Polyuria) or R39.1 (Other and unspecified difficulties with micturition). These codes are used when a more specific diagnosis hasn’t been established yet. It is important to note that these codes are not specific to frequency alone and may encompass other urinary symptoms.
- R35: Polyuria. This code indicates excessive urination. While not solely focused on frequency, it can be used when the patient is producing an abnormally large volume of urine, leading to frequent trips to the bathroom.
- R39.1: Other and unspecified difficulties with micturition. This is a broader code that can be applied when the patient is experiencing problems with urination, including frequency, urgency, or hesitancy, and a more specific diagnosis is not yet available.
It’s important to note that these are just examples, and the appropriate code will depend on the specific clinical scenario. For example, if the urinary frequency is due to a urinary tract infection (UTI), the ICD-10 code for the UTI would be used (e.g., N39.0 for Urinary tract infection, site not specified). If it’s related to an enlarged prostate (benign prostatic hyperplasia or BPH), the code N40 would be relevant. Furthermore, conditions such as diabetes mellitus (E08-E13) can cause polyuria and secondary urinary frequency, and the appropriate diabetes code would be used with additional codes for any related complications.
Factors Influencing the Choice of ICD-10 Code
Selecting the correct ICD-10 code requires careful consideration of several factors:
- Underlying Cause: The primary driver for code selection is the underlying cause of the urinary frequency. A UTI will have a different code than BPH or diabetes.
- Associated Symptoms: Are there other symptoms present, such as pain, burning, urgency, or incontinence? These will influence the code selection.
- Diagnostic Findings: Results from urine tests, blood tests, imaging studies, and other diagnostic procedures are crucial for determining the correct diagnosis and ICD-10 code.
- Medical History: The patient’s past medical history, including any relevant conditions or medications, should be taken into account.
- Provider Documentation: Accurate and detailed documentation by the healthcare provider is essential for proper coding.
The Role of Accurate Coding in Healthcare
Accurate ICD-10 coding is vital for several reasons:
- Proper Reimbursement: Correct coding ensures that healthcare providers receive appropriate reimbursement for the services they provide.
- Data Analysis and Research: ICD-10 data is used for tracking disease prevalence, identifying trends, and conducting research.
- Public Health Monitoring: Accurate coding helps public health agencies monitor and respond to health threats.
- Quality Improvement: ICD-10 data can be used to identify areas for improvement in healthcare delivery.
Inaccurate coding can lead to claim denials, underpayment, or even legal issues. It can also skew data and hinder research efforts. Therefore, it is crucial for healthcare providers and coders to stay up-to-date on the latest ICD-10 guidelines and coding conventions.
Urinary Frequency and Potential Underlying Conditions
Urinary frequency is a symptom that can stem from a multitude of underlying conditions. Understanding these potential causes is crucial for both diagnosis and treatment. Some of the more common conditions associated with urinary frequency include:
- Urinary Tract Infection (UTI): UTIs are a frequent cause of urinary frequency, especially in women. The infection irritates the bladder, leading to a frequent urge to urinate.
- Overactive Bladder (OAB): OAB is a condition in which the bladder muscles contract involuntarily, causing a sudden and frequent urge to urinate.
- Diabetes: Both type 1 and type 2 diabetes can lead to increased thirst and urination. High blood sugar levels cause the kidneys to work harder to filter out excess glucose, resulting in frequent urination.
- Benign Prostatic Hyperplasia (BPH): In men, an enlarged prostate can press on the urethra, causing urinary frequency, urgency, and difficulty emptying the bladder.
- Interstitial Cystitis (IC): IC, also known as painful bladder syndrome, is a chronic condition that causes bladder pain, pressure, and urinary frequency.
- Diuretics: Certain medications, such as diuretics (water pills), can increase urine production and lead to urinary frequency.
- Pregnancy: During pregnancy, hormonal changes and the growing uterus can put pressure on the bladder, causing urinary frequency.
- Neurological Conditions: Conditions such as multiple sclerosis (MS), Parkinson’s disease, and stroke can affect bladder control and lead to urinary frequency.
It’s important to consult with a healthcare professional to determine the underlying cause of urinary frequency and receive appropriate treatment.
The Diagnostic Process for Urinary Frequency
Diagnosing the cause of urinary frequency typically involves a comprehensive evaluation, including:
- Medical History: The healthcare provider will ask about the patient’s medical history, including any relevant conditions, medications, and symptoms.
- Physical Exam: A physical exam may be performed to assess the patient’s overall health and identify any potential underlying causes.
- Urine Tests: Urine tests, such as urinalysis and urine culture, can help detect infection, blood, or other abnormalities in the urine.
- Bladder Diary: The patient may be asked to keep a bladder diary to track their urination habits, including frequency, volume, and any associated symptoms.
- Postvoid Residual (PVR) Measurement: A PVR measurement assesses the amount of urine remaining in the bladder after urination.
- Urodynamic Testing: Urodynamic testing evaluates bladder function and can help identify problems with bladder storage or emptying.
- Cystoscopy: Cystoscopy is a procedure in which a thin, flexible tube with a camera is inserted into the bladder to visualize the bladder lining.
The specific diagnostic tests performed will depend on the patient’s individual circumstances and the healthcare provider’s clinical judgment. Based on the results of these tests, the healthcare provider can determine the underlying cause of the urinary frequency and develop an appropriate treatment plan.
Treatment Options for Urinary Frequency
Treatment for urinary frequency depends on the underlying cause. Some common treatment options include:
- Antibiotics: If the urinary frequency is caused by a UTI, antibiotics will be prescribed to clear the infection.
- Medications for Overactive Bladder: Medications such as anticholinergics and beta-3 agonists can help relax the bladder muscles and reduce urinary frequency and urgency.
- Lifestyle Modifications: Lifestyle modifications, such as limiting caffeine and alcohol intake, can help reduce bladder irritation and urinary frequency.
- Bladder Training: Bladder training involves gradually increasing the time between trips to the bathroom to help increase bladder capacity.
- Pelvic Floor Exercises: Pelvic floor exercises, also known as Kegel exercises, can help strengthen the pelvic floor muscles and improve bladder control.
- Surgery: In some cases, surgery may be necessary to treat underlying conditions such as BPH or interstitial cystitis.
It’s important to work with a healthcare professional to develop a treatment plan that is tailored to your individual needs and circumstances.
The Importance of Seeking Medical Attention
While urinary frequency can sometimes be a minor inconvenience, it can also be a sign of a more serious underlying condition. It’s important to seek medical attention if you experience:
- Sudden or severe urinary frequency
- Urinary frequency accompanied by pain, burning, or fever
- Blood in the urine
- Difficulty urinating
- Loss of bladder control
These symptoms could indicate a serious infection, kidney problems, or other medical conditions that require prompt treatment. Early diagnosis and treatment can help prevent complications and improve your overall health.
Advancements in Diagnostic and Treatment Approaches
The field of urology is constantly evolving, with new diagnostic and treatment approaches emerging regularly. Some recent advancements include:
- Advanced Imaging Techniques: Advanced imaging techniques, such as MRI and CT scans, can provide detailed images of the urinary tract and help identify underlying causes of urinary frequency.
- Minimally Invasive Surgical Procedures: Minimally invasive surgical procedures, such as robotic surgery and laparoscopy, can be used to treat conditions such as BPH and bladder cancer with less pain and a shorter recovery time.
- New Medications: New medications are being developed to treat overactive bladder and other urinary conditions with fewer side effects.
- Neuromodulation Therapies: Neuromodulation therapies, such as sacral nerve stimulation, can help regulate bladder function and reduce urinary frequency and urgency.
These advancements offer hope for individuals suffering from urinary frequency and other urinary problems.
Living Comfortably with Urinary Frequency
Living with urinary frequency can be challenging, but there are steps you can take to manage your symptoms and improve your quality of life:
- Maintain a healthy lifestyle: Eat a balanced diet, exercise regularly, and get enough sleep.
- Avoid bladder irritants: Limit your intake of caffeine, alcohol, and acidic foods.
- Stay hydrated: Drink plenty of water throughout the day, but avoid drinking large amounts of fluids before bedtime.
- Practice good bladder habits: Urinate regularly and try to empty your bladder completely each time.
- Manage stress: Stress can worsen urinary frequency. Practice relaxation techniques such as yoga or meditation.
- Wear comfortable clothing: Avoid tight clothing that can put pressure on your bladder.
By following these tips, you can take control of your symptoms and live a more comfortable and fulfilling life.
Expert Insights on Managing Urinary Frequency
We consulted with Dr. Sarah Miller, a leading urologist, to gather her insights on managing urinary frequency. According to Dr. Miller, “The key to effectively managing urinary frequency is to identify and treat the underlying cause. A thorough evaluation, including a detailed medical history, physical exam, and appropriate diagnostic tests, is essential for determining the correct diagnosis and developing an individualized treatment plan.”
Dr. Miller also emphasizes the importance of lifestyle modifications. “Simple changes to your diet and fluid intake can often make a significant difference in reducing urinary frequency. Limiting caffeine and alcohol, staying hydrated, and practicing good bladder habits are all important steps to take.”
Finally, Dr. Miller stresses the importance of seeking medical attention if you experience any concerning symptoms. “Don’t hesitate to see a healthcare professional if you have sudden or severe urinary frequency, pain, burning, or blood in your urine. Early diagnosis and treatment can help prevent complications and improve your overall health.”
Navigating the ICD-10 Coding Landscape
The ICD-10 coding system can be complex and challenging to navigate. Here are some tips for ensuring accurate coding:
- Stay up-to-date on the latest guidelines: The ICD-10 coding guidelines are updated annually by the CDC and CMS. Stay informed about any changes or revisions.
- Use coding resources: Utilize coding manuals, online resources, and coding software to assist with code selection.
- Seek clarification when needed: If you are unsure about the correct code to use, consult with a certified coder or coding expert.
- Document thoroughly: Accurate and detailed documentation by the healthcare provider is essential for proper coding.
- Participate in coding training: Attend coding workshops and seminars to enhance your knowledge and skills.
By following these tips, you can ensure that your coding is accurate, compliant, and effective.
Understanding the Broader Implications
Understanding the ICD-10 code related to urinary frequency extends beyond mere coding accuracy. It touches upon patient care, data analysis, and public health initiatives. Correctly identifying and coding urinary frequency allows for better tracking of related conditions, resource allocation for treatment, and ultimately, improved patient outcomes. The data gathered from ICD-10 coding informs research, helps identify trends, and allows healthcare providers to tailor their approach to patient care. It’s a cornerstone of modern healthcare management and a crucial tool for understanding and addressing common health concerns.
Moving Forward: Taking Control of Your Urinary Health
Understanding the nuances of the ICD-10 code for urinary frequency is just the first step. Recognizing the potential underlying causes, seeking timely medical attention, and adopting healthy lifestyle habits are crucial for managing this condition effectively. By working closely with your healthcare provider, you can develop a personalized treatment plan that addresses your specific needs and helps you regain control of your urinary health. We encourage you to share your experiences with urinary frequency in the comments below to support others navigating similar challenges.
