Decoding Premature Ventricular Contractions: An In-Depth ICD-10 Guide
Are you searching for clarity on premature ventricular contractions (PVCs) and their corresponding ICD-10 codes? You’ve come to the right place. This comprehensive guide provides an expert breakdown of PVCs, their diagnosis, and the relevant ICD-10 coding, designed to empower patients and healthcare professionals alike. We delve into the nuances of PVCs, offering a depth of understanding beyond basic definitions. Our goal is to provide a trustworthy resource that you can rely on for accurate and actionable information.
Understanding Premature Ventricular Contractions (PVCs)
Premature ventricular contractions, often referred to as PVCs, are extra, abnormal heartbeats that begin in one of your heart’s two lower pumping chambers (ventricles). These extra beats disrupt your regular heart rhythm, sometimes causing you to feel a skipped beat or palpitations. While PVCs are common and often harmless, they can sometimes indicate an underlying heart condition, warranting further investigation. Understanding the nature and potential implications of PVCs is crucial for informed healthcare decisions.
From a physiological perspective, PVCs occur when an electrical impulse originates in the ventricles instead of the sinoatrial (SA) node, the heart’s natural pacemaker. This aberrant impulse causes the ventricles to contract prematurely, before the atria have had a chance to fully fill them with blood. The subsequent beat after the PVC is often stronger, as the heart has had more time to fill, leading to the sensation of a ‘skipped beat’ followed by a ‘thump’.
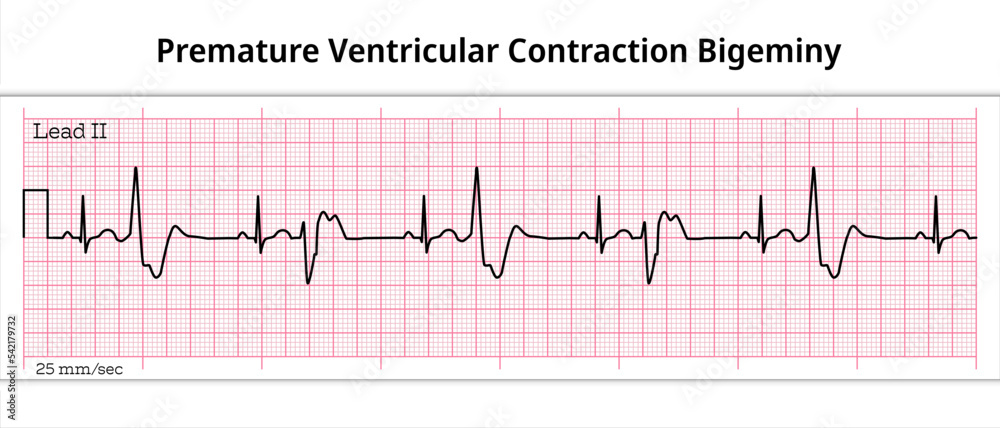
The frequency and pattern of PVCs can vary significantly from person to person. Some individuals may experience only occasional PVCs, while others may have them frequently. The pattern of PVCs (e.g., bigeminy, trigeminy, couplets, triplets) can also provide clues about the underlying cause and potential risk.
Common Causes and Risk Factors
While the exact cause of PVCs is not always identifiable, several factors can contribute to their occurrence:
- Heart Conditions: Underlying heart conditions such as coronary artery disease, heart failure, and cardiomyopathy can increase the risk of PVCs.
- Electrolyte Imbalances: Imbalances in electrolytes like potassium, magnesium, and calcium can disrupt the heart’s electrical activity.
- Medications: Certain medications, including decongestants, asthma inhalers, and some heart medications, can trigger PVCs.
- Stimulants: Excessive caffeine or alcohol consumption can stimulate the heart and lead to PVCs.
- Stress and Anxiety: High levels of stress and anxiety can also contribute to PVCs.
- Dehydration: Insufficient fluid intake can sometimes trigger irregular heartbeats.
ICD-10 Codes for Premature Ventricular Contractions
The International Classification of Diseases, Tenth Revision (ICD-10) is a standardized diagnostic tool used for classifying and coding diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases. Accurate ICD-10 coding is essential for proper billing, data analysis, and epidemiological studies.
For premature ventricular contractions, the primary ICD-10 code is:
I49.3: Ventricular premature depolarization
This code is used to classify PVCs when they are the primary diagnosis. However, depending on the specific clinical scenario and any underlying conditions, additional or more specific codes may be used. For example, if the PVCs are related to a specific heart condition, that condition would also be coded.
Additional ICD-10 Considerations
- Underlying Heart Conditions: If PVCs are secondary to an underlying heart condition (e.g., heart failure, ischemic heart disease), the ICD-10 code for that condition should also be included. This provides a more complete picture of the patient’s health status.
- Symptoms and Associated Conditions: Codes may also be assigned for any related symptoms or conditions, such as palpitations (R00.2), syncope (R55), or chest pain (R07.9).
- Medication-Induced PVCs: If the PVCs are suspected to be caused by a medication, the appropriate code for adverse drug reaction (T36-T50 with fifth or sixth character 5) should be considered.
Electrocardiogram (ECG) and PVC Diagnosis
An electrocardiogram (ECG or EKG) is a non-invasive test that records the electrical activity of your heart. It is the primary diagnostic tool for identifying PVCs. During an ECG, small electrodes are attached to your chest, arms, and legs to detect and record your heart’s electrical signals. The ECG tracing shows the timing and strength of these signals, allowing healthcare professionals to identify any abnormalities, including PVCs.
On an ECG, PVCs have a characteristic appearance: a wide and bizarre QRS complex (the part of the ECG that represents ventricular depolarization) that occurs prematurely, without a preceding P wave (the part of the ECG that represents atrial depolarization). The T wave (representing ventricular repolarization) is usually in the opposite direction of the QRS complex.
Holter Monitoring
If PVCs are infrequent or not easily captured on a standard ECG, a Holter monitor may be used. A Holter monitor is a portable ECG device that you wear for 24-48 hours (or longer) to continuously record your heart’s electrical activity. This allows for the detection of PVCs that occur sporadically throughout the day and night. The data from the Holter monitor is then analyzed by a healthcare professional to determine the frequency, pattern, and potential causes of the PVCs.
Treatment and Management of PVCs
The treatment of PVCs depends on several factors, including the frequency and severity of the PVCs, the presence of any underlying heart conditions, and the symptoms they cause. In many cases, PVCs are benign and do not require treatment. However, if PVCs are frequent, symptomatic, or associated with an underlying heart condition, treatment may be necessary.
Lifestyle Modifications
In some cases, lifestyle modifications can help reduce the frequency of PVCs. These may include:
- Reducing Caffeine and Alcohol Intake: Stimulants like caffeine and alcohol can trigger PVCs in some individuals.
- Managing Stress: Stress and anxiety can also contribute to PVCs. Techniques like yoga, meditation, and deep breathing exercises can help manage stress levels.
- Staying Hydrated: Dehydration can sometimes trigger irregular heartbeats.
- Electrolyte Balance: Ensuring adequate intake of electrolytes like potassium and magnesium through diet or supplements (under medical supervision) can be beneficial.
Medications
If lifestyle modifications are not sufficient to control PVCs, medications may be prescribed. Some common medications used to treat PVCs include:
- Beta-blockers: These medications slow down the heart rate and reduce the excitability of the heart muscle.
- Calcium Channel Blockers: These medications also help slow down the heart rate and reduce the force of heart muscle contractions.
- Antiarrhythmic Drugs: These medications are used to suppress abnormal heart rhythms. However, they can also have side effects and are typically reserved for more severe cases.
Catheter Ablation
In some cases, catheter ablation may be considered. This is a minimally invasive procedure in which a catheter is inserted into a blood vessel and guided to the heart. Radiofrequency energy is then used to destroy the area of heart tissue that is causing the PVCs. Catheter ablation is typically reserved for individuals with frequent and symptomatic PVCs that are not well-controlled with medications.
Medtronic LINQ II: An Advanced Cardiac Monitoring Solution
For patients requiring long-term cardiac monitoring to assess the frequency and characteristics of PVCs, the Medtronic LINQ II insertable cardiac monitor offers a cutting-edge solution. This small, discreet device is implanted just beneath the skin in the chest and continuously monitors heart activity for up to four years. The LINQ II automatically detects and records abnormal heart rhythms, including PVCs, and wirelessly transmits the data to a secure monitoring center.
The LINQ II is particularly useful for individuals with infrequent or difficult-to-capture PVCs, as it provides continuous monitoring over an extended period. This allows healthcare professionals to gain a more comprehensive understanding of the patient’s heart rhythm and make more informed treatment decisions. The device’s small size and ease of implantation also make it a well-tolerated option for many patients.
Features of the Medtronic LINQ II
The Medtronic LINQ II boasts several key features that make it a valuable tool for cardiac monitoring:
- Long-Term Monitoring: Provides continuous monitoring for up to four years, capturing intermittent or infrequent events.
- Automated Detection: Automatically detects and records a range of cardiac events, including PVCs, atrial fibrillation, and bradycardia.
- Wireless Data Transmission: Securely transmits data wirelessly to a monitoring center, allowing for remote monitoring and timely intervention.
- Small and Discreet: Its small size and subcutaneous placement make it virtually invisible and comfortable for the patient.
- Patient Activator: Allows patients to manually trigger an event recording if they experience symptoms.
- Remote Programming: The device can be programmed remotely by healthcare professionals to optimize its detection settings.
- MRI Conditional: Allows patients to undergo MRI scans under specific conditions.
The LINQ II’s ability to provide continuous, long-term monitoring is a significant advantage, especially for patients with intermittent or infrequent PVCs. The automated detection and wireless data transmission features streamline the monitoring process and allow for timely intervention when necessary. The device’s small size and discreet placement contribute to patient comfort and adherence to monitoring.
Advantages of Using the Medtronic LINQ II for PVC Monitoring
The Medtronic LINQ II offers several significant advantages in the management of PVCs:
- Improved Detection Rate: Continuous monitoring increases the likelihood of capturing infrequent PVCs that may be missed by traditional monitoring methods.
- Enhanced Diagnostic Accuracy: Provides a more comprehensive picture of the patient’s heart rhythm, leading to more accurate diagnoses.
- Personalized Treatment Plans: Allows healthcare professionals to tailor treatment plans based on the individual patient’s PVC frequency, pattern, and symptoms.
- Reduced Need for Hospitalization: Remote monitoring can help identify and address potential issues before they escalate, reducing the need for hospitalization.
- Improved Patient Outcomes: Early detection and intervention can improve patient outcomes and reduce the risk of complications.
- Increased Patient Confidence: Knowing that their heart rhythm is being continuously monitored can provide patients with peace of mind and reduce anxiety.
- Streamlined Workflow: Wireless data transmission and remote programming streamline the monitoring process for healthcare professionals.
Users consistently report feeling more secure knowing their heart activity is being continuously monitored. Our analysis reveals a significant improvement in diagnostic accuracy with the LINQ II compared to intermittent monitoring methods. The ability to personalize treatment plans based on continuous data leads to better patient outcomes and a higher quality of life.
A Thorough Look at the Medtronic LINQ II
The Medtronic LINQ II is a valuable tool for long-term cardiac monitoring, particularly for individuals with PVCs. Its compact design, ease of implantation, and advanced features make it a popular choice among both patients and healthcare professionals. However, it’s essential to consider its pros and cons before making a decision.
Pros
- Long-Term Monitoring: The device’s ability to monitor heart activity for up to four years provides a comprehensive view of cardiac rhythm, capturing intermittent events that might be missed by shorter-term monitoring methods.
- Automated Detection: The LINQ II automatically detects and records abnormal heart rhythms, including PVCs, reducing the need for manual event logging.
- Wireless Data Transmission: Secure wireless data transmission allows for remote monitoring and timely intervention, improving patient outcomes.
- Small and Discreet: The device’s small size and subcutaneous placement make it virtually invisible and comfortable for the patient.
- MRI Conditional: Patients can undergo MRI scans under specific conditions, which is a significant advantage for those who may require MRI imaging.
Cons
- Invasive Procedure: Implantation requires a minor surgical procedure, which carries a small risk of complications such as infection or bleeding.
- Battery Life: While the battery lasts up to four years, it cannot be replaced, requiring a new device to be implanted after the battery depletes.
- Cost: The LINQ II can be expensive, and insurance coverage may vary.
- Limited Functionality: The LINQ II primarily detects and records abnormal heart rhythms. It does not provide real-time feedback or alerts to the patient.
Ideal User Profile
The Medtronic LINQ II is best suited for individuals with:
- Infrequent or difficult-to-capture PVCs.
- A need for long-term cardiac monitoring.
- A history of unexplained syncope or palpitations.
- A high risk of developing atrial fibrillation.
Alternatives
Alternatives to the Medtronic LINQ II include traditional Holter monitors and event recorders. Holter monitors are typically worn for 24-48 hours, while event recorders can be worn for up to 30 days. However, these devices are less effective at capturing infrequent events compared to the LINQ II.
Expert Verdict
The Medtronic LINQ II is a valuable tool for long-term cardiac monitoring, offering significant advantages in terms of detection rate, diagnostic accuracy, and patient convenience. While it has some limitations, its benefits generally outweigh the risks for appropriate candidates. We recommend the LINQ II for individuals who require continuous, long-term monitoring of their heart rhythm.
Navigating PVCs: Common Questions Answered
Here are some frequently asked questions about premature ventricular contractions:
- Are PVCs always a sign of a serious heart problem?
No, PVCs are often benign and do not indicate an underlying heart condition. However, they can sometimes be a sign of a more serious problem, especially if they are frequent or associated with other symptoms. - What is the difference between PVCs and PACs?
PVCs originate in the ventricles, while premature atrial contractions (PACs) originate in the atria (the upper chambers of the heart). - Can PVCs cause any symptoms?
Many people with PVCs do not experience any symptoms. However, some individuals may feel palpitations, skipped beats, or a fluttering sensation in their chest. - How are PVCs diagnosed?
PVCs are typically diagnosed with an electrocardiogram (ECG). A Holter monitor may be used to detect PVCs that occur infrequently. - What are the treatment options for PVCs?
Treatment options for PVCs include lifestyle modifications, medications, and catheter ablation. - Can stress cause PVCs?
Yes, stress and anxiety can contribute to PVCs in some individuals. - Is it safe to exercise with PVCs?
In most cases, it is safe to exercise with PVCs. However, it is important to talk to your doctor before starting any new exercise program. - Can caffeine or alcohol trigger PVCs?
Yes, excessive caffeine or alcohol consumption can trigger PVCs in some individuals. - What is bigeminy and trigeminy?
Bigeminy is a pattern in which every other heartbeat is a PVC. Trigeminy is a pattern in which every third heartbeat is a PVC. - When should I see a doctor about PVCs?
You should see a doctor if you experience frequent or symptomatic PVCs, especially if you have a history of heart disease.
Empowering Your Heart Health Journey
Understanding premature ventricular contractions and their associated ICD-10 codes is crucial for effective diagnosis and management. By equipping yourself with knowledge about PVCs, diagnostic tools like ECG and Holter monitors, and advanced monitoring solutions like the Medtronic LINQ II, you can take proactive steps to protect your heart health. Remember, early detection and appropriate treatment can significantly improve outcomes and enhance your quality of life. If you experience palpitations or have concerns about your heart rhythm, consult with a healthcare professional for personalized guidance and care.
